We practice a minimally invasive approach to your foot or ankle problem with surgery as the last option
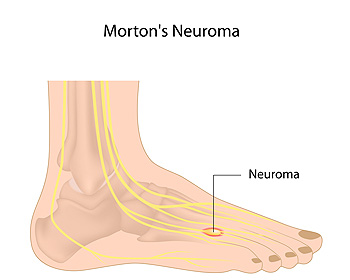 Morton’s neuroma is a condition which causes swelling along a nerve in the foot. The affected nerve is typically between the third and fourth toes, or the second and third toes. The symptoms of this condition include tingling, burning, numbness, pain, and the sensation that you are stepping on something inside your shoe. Symptoms typically begin gradually, often while wearing narrow shoes or performing certain physical activities, and go away with rest. However, as the condition progresses, the symptoms may worsen and persist for days or even weeks as the swelling along the nerve enlarges. If you are experiencing the symptoms of Morton’s neuroma, it is recommended that you seek the care of a podiatrist.
Morton’s neuroma is a condition which causes swelling along a nerve in the foot. The affected nerve is typically between the third and fourth toes, or the second and third toes. The symptoms of this condition include tingling, burning, numbness, pain, and the sensation that you are stepping on something inside your shoe. Symptoms typically begin gradually, often while wearing narrow shoes or performing certain physical activities, and go away with rest. However, as the condition progresses, the symptoms may worsen and persist for days or even weeks as the swelling along the nerve enlarges. If you are experiencing the symptoms of Morton’s neuroma, it is recommended that you seek the care of a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. David Ungar of Personal Foot Care. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
 The condition that is referred to as cracked heels can be uncomfortable. In severe cases, where the cracks in the skin are deep, bleeding may occur. These are known as fissures and may become infected if not promptly treated. There are several reasons for this condition to develop that include being obese, standing for long periods of time on hard surfaces, and wearing shoes that have an open back. Mild relief may be felt when the affected heel is washed and dried thoroughly, followed by using a good moisturizer. If you have cracked heels, it is suggested that you speak with a podiatrist who can effectively treat this condition.
The condition that is referred to as cracked heels can be uncomfortable. In severe cases, where the cracks in the skin are deep, bleeding may occur. These are known as fissures and may become infected if not promptly treated. There are several reasons for this condition to develop that include being obese, standing for long periods of time on hard surfaces, and wearing shoes that have an open back. Mild relief may be felt when the affected heel is washed and dried thoroughly, followed by using a good moisturizer. If you have cracked heels, it is suggested that you speak with a podiatrist who can effectively treat this condition.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Dr. David Ungar from Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
Ways to Prevent Cracked Heels
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
 People who regularly stretch their feet are often aware of the benefits that can come from frequently practicing foot stretches. An effective way to stretch the Achilles tendon is done by standing on a step, and gently lowering one foot at a time. The big toe can be stretched by grasping the heel while sitting down, and slowly bending the big toe toward you. Additionally, this is helpful in stretching the sole of the foot. The toes can become stronger when a towel curl stretch is performed. This is practiced by placing your foot on a towel, and gently grabbing it with your toes. For more information about the benefits of stretching the feet, please schedule an appointment with a podiatrist.
People who regularly stretch their feet are often aware of the benefits that can come from frequently practicing foot stretches. An effective way to stretch the Achilles tendon is done by standing on a step, and gently lowering one foot at a time. The big toe can be stretched by grasping the heel while sitting down, and slowly bending the big toe toward you. Additionally, this is helpful in stretching the sole of the foot. The toes can become stronger when a towel curl stretch is performed. This is practiced by placing your foot on a towel, and gently grabbing it with your toes. For more information about the benefits of stretching the feet, please schedule an appointment with a podiatrist.
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Dr. David Ungar from Personal Foot Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising and ice and rest the foot. It is advised to then see a podiatrist for help.
If you have any questions, please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
 Patients who have diabetes may be aware of the importance of properly caring for their feet. This can help to prevent the painful condition that is known as a diabetic foot ulcer. This type of wound may develop as a result of the inability of feeling a small cut on the foot, and it may quickly become infected. This can happen from elevated glucose levels in the blood, which may hinder the body’s capability to heal properly. Mild relief and proper healing may come from keeping weight off of the foot, and it may help to elevate it often. It is imperative that proper dressings are used as the healing process takes place, in addition to keeping the foot as clean and as dry as possible. If you have diabetes, it is strongly suggested that you seek the counsel of a podiatrist who can properly treat this condition.
Patients who have diabetes may be aware of the importance of properly caring for their feet. This can help to prevent the painful condition that is known as a diabetic foot ulcer. This type of wound may develop as a result of the inability of feeling a small cut on the foot, and it may quickly become infected. This can happen from elevated glucose levels in the blood, which may hinder the body’s capability to heal properly. Mild relief and proper healing may come from keeping weight off of the foot, and it may help to elevate it often. It is imperative that proper dressings are used as the healing process takes place, in addition to keeping the foot as clean and as dry as possible. If you have diabetes, it is strongly suggested that you seek the counsel of a podiatrist who can properly treat this condition.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Dr. David Ungar from Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetes is the condition in which the body does not properly process food for use as energy. People with Type 1 diabetes cannot produce insulin, which is required for glucose to feed your body’s cells. It is typically caused by the immune system mistaking healthy cells for foreign invaders and destroying the insulin-producing cells in the pancreas. On the other hand, people with Type 2 diabetes cannot respond to insulin properly, and eventually cannot produce enough. The Centers for Disease Control and Prevention reports that over 30 million people in the United States have diabetes, with 1 in 4 having no idea they have it. Surprisingly, diabetes is the seventh leading cause of death in the US. The symptoms of diabetes include frequent urination, fatigue, hunger, and even blurry vision.
Diabetes can also affect the feet as well. Over time, diabetes can cause nerve damage to your feet, which could then lead to symptoms such as tingling, pain and numbness in the feet. Neuropathy can be very dangerous to a person with diabetes, since it prevents them from feeling injuries such as cuts or blisters in the feet, and if not detected early enough, may lead to infection. Neuropathy can also lead changes in the shape of your feet and toes. The best way for people with diabetes to prevent or delay neuropathy is keeping their blood glucose levels in their target range. This consists of eating right, having the correct amount of exercise, and taking medications.
Diabetes can also create calluses and foot ulcers as well. Calluses build up faster and occur more frequently with those affected by diabetes. If there are too many calluses, therapeutic shoes and inserts may be required. It is important to have calluses trimmed by a health professional, as doing it yourself may lead to infections. If these calluses continue to develop and thicken, they can lead to foot ulcers. Foot ulcers are open sores, that appear on the ball of the foot or on the bottom of the big toe. These ulcers can lead to future infections if not treated and may possibly result in losing a limb. It is important to report any ulcers to your podiatrist right away. Your doctor may take x-rays to examine the foot and clean out any dead and infected tissue.
Lastly, diabetes can also lead to poor circulation and peripheral arterial disease (PAD). The poor circulation in the feet and leg area is a result of diabetes narrowing and hardening, eventually slowing down the blood flow in that area. The best way to prevent this is to keep away from smoking and follow your doctor’s advice for maintaining blood pressure and cholesterol. PAD is similar to this complication. PAD is when blood vessels narrow or are blocked by fatty deposits. PAD also increases your risk of heart attacks and strokes and is a common condition to those affected by diabetes. The combination of both PAD and neuropathy may lead to infections and can result in amputation of certain limbs. PAD can be prevented with wearing the proper foot wear and regularly taking care of your feet.
If you want to take care of your feet, you should wash and dry them carefully and perform daily inspections to check for cuts, blisters, or swelling. Any physical activity you partake in should be approved by your health care provider. You should also be sure to wear special shoes if advised to do so by your doctor.
 A hairline fracture that gradually occurs may be defined as a stress fracture. It can happen as a result of frequently running or participating in sporting activities, and is known to develop from overuse. If a stress fracture is not promptly treated, it will typically get worse as the activity continues. The common symptoms that are associated with this condition may include swelling, pain and discomfort surrounding the affected area, and it may be difficult to walk. Factors that may lead to the development of a stress fracture can consist of wearing shoes that do not fit correctly, running on hard or uneven surfaces, or existing medical conditions such as osteoporosis. Relief may be obtained by elevating the affected foot, as this may help to reduce swelling. If you have endured a stress fracture it is suggested that you schedule a consultation with a podiatrist as quickly as possible, so proper treatment can begin.
A hairline fracture that gradually occurs may be defined as a stress fracture. It can happen as a result of frequently running or participating in sporting activities, and is known to develop from overuse. If a stress fracture is not promptly treated, it will typically get worse as the activity continues. The common symptoms that are associated with this condition may include swelling, pain and discomfort surrounding the affected area, and it may be difficult to walk. Factors that may lead to the development of a stress fracture can consist of wearing shoes that do not fit correctly, running on hard or uneven surfaces, or existing medical conditions such as osteoporosis. Relief may be obtained by elevating the affected foot, as this may help to reduce swelling. If you have endured a stress fracture it is suggested that you schedule a consultation with a podiatrist as quickly as possible, so proper treatment can begin.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Dr. David Ungar from Personal Foot Care. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
 An ingrown toenail is an uncomfortable condition that generally affects the big toe. It occurs as a result of the toenail growing into the outer edges of the skin. Typical symptoms that many patients notice with this ailment can include redness, swelling, pain, and discomfort. Moderate relief may be found if larger shoes are worn as the healing process takes place, in addition to soaking the affected toe in warm water. In severe cases, the nail may become infected, and surgery may be required for proper healing. If you have an ingrown toenail, it is strongly advised that you consult with a podiatrist as quickly as possible to obtain the best treatment for your condition.
An ingrown toenail is an uncomfortable condition that generally affects the big toe. It occurs as a result of the toenail growing into the outer edges of the skin. Typical symptoms that many patients notice with this ailment can include redness, swelling, pain, and discomfort. Moderate relief may be found if larger shoes are worn as the healing process takes place, in addition to soaking the affected toe in warm water. In severe cases, the nail may become infected, and surgery may be required for proper healing. If you have an ingrown toenail, it is strongly advised that you consult with a podiatrist as quickly as possible to obtain the best treatment for your condition.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Dr. David Ungar of Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
 Research has indicated that approximately half of the population is affected with nail fungus, and it is most likely to occur in the toenails. It is caused by a fungal infection, and typically develops in the big toe. There are several symptoms that are associated with this ailment. These can include a yellowing of the nail, and it may appear brittle and dull. In severe cases, the nail may produce a foul odor, and can lift from the nail bed. The fungus that causes this contagious condition lives and thrives in warm and moist areas. These can consist of public swimming pools and locker room floors. There may be preventive measures that can be taken that can include wearing appropriate shoes while in these types of environments, in addition to wearing shoes and socks that are made of a breathable material. If you notice a toenail fungus is developing, it is suggested that you schedule a consultation with a podiatrist who can offer you proper treatment techniques.
Research has indicated that approximately half of the population is affected with nail fungus, and it is most likely to occur in the toenails. It is caused by a fungal infection, and typically develops in the big toe. There are several symptoms that are associated with this ailment. These can include a yellowing of the nail, and it may appear brittle and dull. In severe cases, the nail may produce a foul odor, and can lift from the nail bed. The fungus that causes this contagious condition lives and thrives in warm and moist areas. These can consist of public swimming pools and locker room floors. There may be preventive measures that can be taken that can include wearing appropriate shoes while in these types of environments, in addition to wearing shoes and socks that are made of a breathable material. If you notice a toenail fungus is developing, it is suggested that you schedule a consultation with a podiatrist who can offer you proper treatment techniques.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Dr. David Ungar of Personal Foot Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Farmington, MI . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Connect With Us
